Paula Orecklin wonders just how many laps around her Winnipeg apartment she has left before the wear on her body takes its toll.
The 32-year-old typically sees a team of health professionals to help keep her symptoms of complex regional pain syndrome -- a chronic condition that causes unrelenting pain in her lower right leg -- under control.
But since the COVID-19 pandemic restricted access to in-person health-care services, Orecklin says her care providers are doing the best they can from afar, but phone appointments just don't have the same depth as going into the doctor's office.
While her pain has abated slightly without the bumpy car rides to physiotherapy, Orecklin says she's been trying to keep up with her exercises while confined to her apartment in an assisted-living facility, but she knows walking in circles around her room is no substitute for her regular sessions.
As a member of the Winnipeg Regional Health Authority's patient and family advisory committee, Orecklin knows plenty of people like her waiting for routine tests and treatments that may not be prioritized in the face of a pandemic, but she fears delaying them will pose health risks in the long run.
"It's not knowing how long I'm going to be able to keep putting things off," Orecklin said. "It's not knowing when I'm going to get my life back."
As authorities across the country have suspended "elective" or "non-essential" health-care services to free up resources for the fight against COVID-19, many patients have seen their appointments cancelled or converted to virtual or phone consultations, and medical procedures postponed.
While these precautions are meant to protect patients from exposure to the novel coronavirus, experts say it can be difficult to determine the threshold of medical urgency in some cases, particularly when the risks of infection are clear, but the potential costs of skipping a checkup are harder to measure.
James Dickinson, a family doctor and professor in University of Calgary's faculty of medicine, said doctors have to make judgement calls that aren't always cut-and-dry.
But now that the novel coronavirus has injected a level of risk into every medical visit, Dickinson said these calculations can be complicated by host of factors.
"There's always a balance of benefits against the harms," Dickinson said. "What's the danger of going out and getting into a health-care setting and possibly getting infected, versus what's the benefit from going there?"
While a healthy individual may be able to skip their regular checkup without issue, Dickinson said the patients who need the most medical attention tend to also be at an increased risk of COVID-19 complications.
These high-risk populations include patients with chronic conditions and people recovering from acute treatment, he said. And within that cohort, there are many "shades of grey" to consider, Dickinson noted.
For example, people with diabetes often undergo a battery of tests every three months. If a patient's results have been consistent for the past year, Dickinson said they can probably wait an extra month or two without much trouble. But if their last tests showed signs of instability, then they may have to come in for another round.
There's also the added layer of difficulty in treating patients remotely, particularly in hands-on fields such as physiotherapy, Dickinson said.
Some patients may see injuries heal on their own, he said. But for others, physiotherapy can go a long way towards alleviating pain and increasing mobility.
Dickinson warned that the ripple effects of these disruptions will only accumulate as the pandemic drags on, and we may not be able to assess the full scope of the damage until we reach the other side.
"There will be tough calls, for all concerned," he said. "There are a few things where it's going to make a big difference."
Jeff Kwong, a family doctor and epidemiologist at University of Toronto's school of public health, said he doesn't see much harm in provinces postponing some preventative tests, such as cancer screenings, for people who seem to be healthy.
But Kwong said if a patient is showing symptoms, then he would still order a diagnostic test to determine treatment.
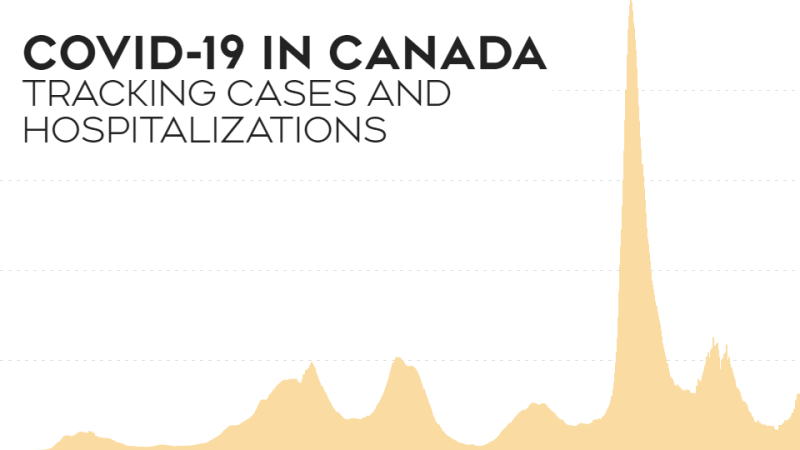
While he acknowledged that delays to routine health care could add up over time, Kwong said medical workers have to focus on the pandemic-sized threat in front of them before they can worry about a possible future backlog of patients.
"There's a small chance that some people could be harmed by this delay," said Kwong. "But I think it's going to be small numbers and the impact will be relatively small compared to a whole bunch of people getting COVID."
Natalie Woods knows that COVID-19 concerns have to take precedence, but with her two-year-old, Tui, growing by the day, she worries delays could have a big impact on her daughter's development.
Tui is hard of hearing, but with the help of hearing aids and a team of health-care professionals, is exploring the full spectrum of sound, Woods said.
But with all of Tui's appointments on hold, Woods is concerned that the toddler will soon outgrow the ear moulds that keep her hearing aids snug.
Many children resist wearing hearing aids, and if Tui goes without them for an extended period, Woods worries she'll get used to "a quieter world" and won't want to turn the volume back up.
At such a critical age, Woods doesn't want all the work Tui has done in learning to listen to go to waste.
"I'm trying to be patient and trust the process," Woods said from her home in Hamilton as Tui babbled nearby.
"But in the back of my mind, especially late at night, I'm worrying about my sweet little girl."
This report by The Canadian Press was first published April 15, 2020.