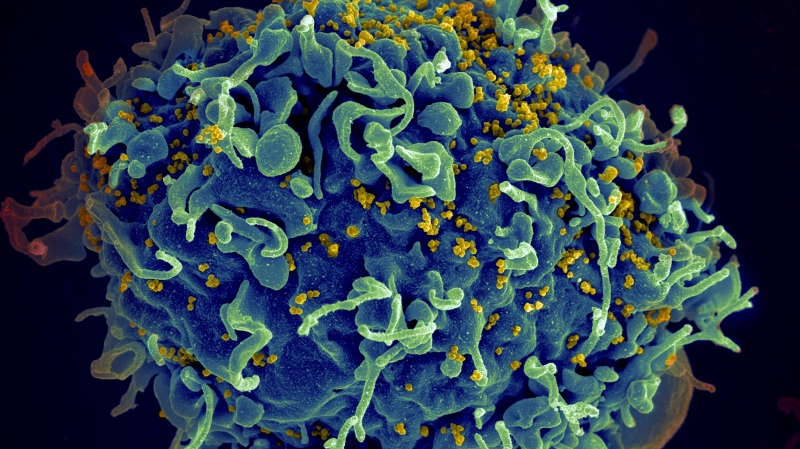
Women have a higher chance of developing long COVID than men, study finds
New research has found that women are "significantly" more likely to suffer from long COVID syndrome compared to men.
The study, conducted by researchers from the Johnson & Johnson Office of the Chief Medical Officer Health of Women Team, found the odds of females developing long COVID is 22 per cent higher than males.
The findings were published Monday, in peer-reviewed journal Current Medical Research and Opinion.
Also known as post-acute COVID-19 syndrome, or PACS for short, long COVID occurs when symptoms linger at least four weeks after the initial recovery period, with some even lasting for months.
While understanding of long COVID is limited, the syndrome can be debilitating and is believed to affect between 10 per cent to one third of those who have been infected.
Previous studies have shown that women are less prone to developing severe disease than men in the acute phase of COVID-19, however, researchers note few studies have assessed sex-differences related to long COVID.
"Knowledge about fundamental sex differences underpinning the clinical manifestations, disease progression, and health outcomes of COVID-19 is crucial for the identification and rational design of effective therapies and public health interventions that are inclusive of and sensitive to the potential differential treatment needs of both sexes," the study's authors wrote.
The latest study found that women with long COVID showed a variety of symptoms including respiratory issues of the ear, nose, and throat, mood and neurological disorders, skin rashes, musculoskeletal pain and fatigue, as well as gastrointestinal and rheumatic disorders.
In comparison, researchers found the men studied were more likely to experience endocrine disorders, such as diabetes and kidney problems.
The study's authors say the findings underscore a "critical need" for sex-disaggregated research, saying the difference in immune system function between females and male "could be an important driver" in developing long COVID.
"Females mount more rapid and robust innate and adaptive immune responses, which can protect them from initial infection and severity. However, this same difference can render females more vulnerable to prolonged autoimmune-related diseases," they wrote.
Researchers analyzed data from about 1.3 million patients compiled from previous studies published between Dec. 2019 and Aug. 2020 on COVID-19, as well as long COVID studies conducted from Jan. 2020 to June 2021.
Of the 640,634 total articles studied, researchers say only 35 provided enough sex-disaggregated data of COVID-19 to examine how females and males differently experience the disease.
While previous studies have looked at sex differences in hospitalizations, ICU admissions and deaths, researchers say the conditions caused by COVID-19 and its long-term impact on the body have been understudied when it comes to females and males.
The study authors note that sex differences in the outcomes of previous coronavirus outbreaks have been reported. Because of this they say the difference between women and men infected with COVID-19 "could have been anticipated."
"Unfortunately, most studies did not evaluate or report granular data by sex, which limited sex-specific clinical insights that may be impacting treatment," they wrote.
Researchers say they hope others build off their findings, looking at additional factors than may impact sex disaggregated data when it comes to COVID-19, such as gender-based disparities in access to care and employment. For example, the study noted that women may be at greater risk of exposure to the virus in certain professions, including nursing and education.
The study's authors say these factors "could affect the natural history of the disease, leading to more complications and sequela," thus more research is needed.
Researchers say having sex disaggregated data is "imperative if we are to ensure that disparate outcomes in disease course are addressed."
CTVNews.ca Top Stories

Trudeau talks border, trade in surprise dinner with Trump at Mar-a-Lago
Prime Minister Justin Trudeau discussed border security and trade during a surprise dinner with U.S.-president elect Donald Trump at Mar-a-Lago in West Palm Beach, Fla. on Friday evening, according to senior government sources.
Man who died trying to help stranded motorist identified as Khalid Farooq, father of 5
The man who lost his life trying to help a stranded motorist Wednesday has been identified as Khalid Farooq.
W5 Investigates 'I never took part in beheadings': Canadian ISIS sniper has warning about future of terror group
An admitted Canadian ISIS sniper held in one of northeast Syria’s highest-security prisons has issued a stark warning about the potential resurgence of the terror group.
Are scented candles bad for you? What the science says
Concerns about the safety of candles are rooted in the chemical reactions that occur when you burn them, as well as in the artificial fragrances and colorants that contribute to the various scents you may love.
Premier League trophy in Toronto as Man City visits Liverpool in high-stakes showdown
Manchester City's Premier League title hopes could hang in the balance Sunday when the slumping club visits league-leading Liverpool.The trophy they are both battling for is 5,450 kilometres away — in Toronto.
Why this Toronto man ran so a giant stickman could dance
Colleagues would ask Duncan McCabe if he was training for a marathon, but, really, the 32-year-old accountant was committing multiple hours of his week, for 10 months, to stylistically run on the same few streets in Toronto's west end with absolutely no race in mind. It was all for the sake of creating a seconds-long animation of a dancing stickman for Strava.
It's time for a good movie this holiday season, here's what's new in theatres
This holiday season has a special edition at the theatres with movies "that everyone has been waiting for," says a movie expert from Ottawa.
Poilievre suggests Trudeau is too weak to engage with Trump, Ford won't go there
While federal Conservative Leader Pierre Poilievre has taken aim at Prime Minister Justin Trudeau this week, calling him too 'weak' to engage with U.S. president-elect Donald Trump, Ontario Premier Doug Ford declined to echo the characterization in an exclusive Canadian broadcast interview set to air this Sunday on CTV's Question Period.
Emboldened 'manosphere' accelerates threats and demeaning language toward women after U.S. election
An emboldened “manosphere” has seized on Republican Donald Trump ’s presidential win to justify misogynistic derision and threats online.
Local Spotlight

Regina's LED volume wall leaving Sask. months after opening
Less than a year after an LED volume wall was introduced to the film world in Saskatchewan, the equipment is making its exit from the province.
'My dear Carmel': Lost letters returned to 103-year-old Guelph, Ont. woman
A young history buff was able to reunite a Guelph, Ont. woman with letters written by her husband almost 80 years ago.
'We have to do something': Homeless advocates in Moncton reaching out for help over holidays
Twice a week, Joanne and Jeff Jonah fill up their vehicle full of snacks and sandwiches and deliver them to the homeless in downtown Moncton, N.B.
100-year-old Winnipeg man walks blocks to see his wife
It's considered lucky to live to be 100, but often when you hit that milestone, you're faced with significant mobility issues. Not Winnipeg's Jack Mudry. The centenarian regularly walks five blocks to get where he wants to go, the care home where his wife Stella lives.
Video shows B.C. cat bursting through pet door to confront raccoons
Several hungry raccoons were chased off a B.C. couple’s deck this week by one over-confident house cat – who was ultimately lucky to saunter away unscathed.
Trailer Park Boys host Canadian premiere of new movie in Dartmouth
Sunday night was a big night for the Trailer Park Boys, as Ricky, Julian and Bubbles hosted an advanced screening of their new movie in Dartmouth, N.S.
Deer spotted wearing high-visibility safety jacket in Northern B.C.
Andrea Arnold is used to having to slow down to let deer cross the road in her Northern B.C. community. But this weekend she saw something that made her pull over and snap a photo.
From cellphones to dentures: Inside Halifax Transit’s lost and found
Every single item misplaced on a bus or ferry in the Halifax Regional Municipality ends up in a small office at the Halifax Transit Bridge Terminal in Dartmouth, N.S.
Torontonians identify priorities, concerns in new city survey
A new public opinion survey has found that 40 per cent of Torontonians don’t feel safe, while half reported that the quality of life in the city has worsened over the last year.