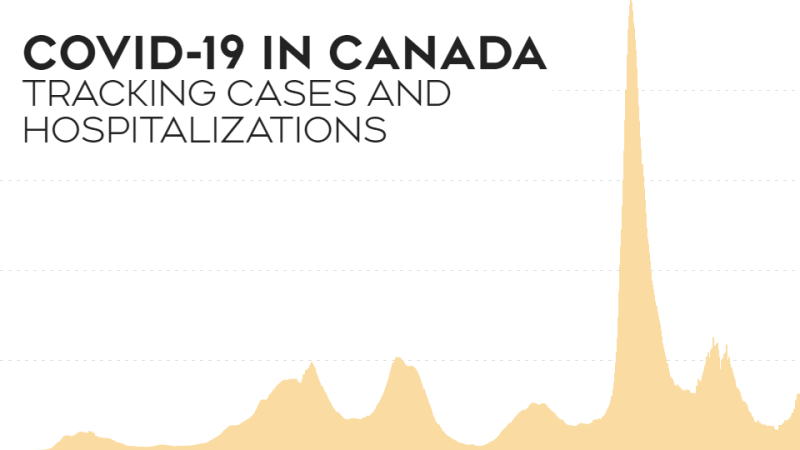
TORONTO -- COVID-19 infections have been rising at an alarming rate for eight consecutive weeks in Canada and abroad — more than 5.2 million new cases were recorded across the globe last week according to the World Health Organization, the most in a single week since the pandemic began.
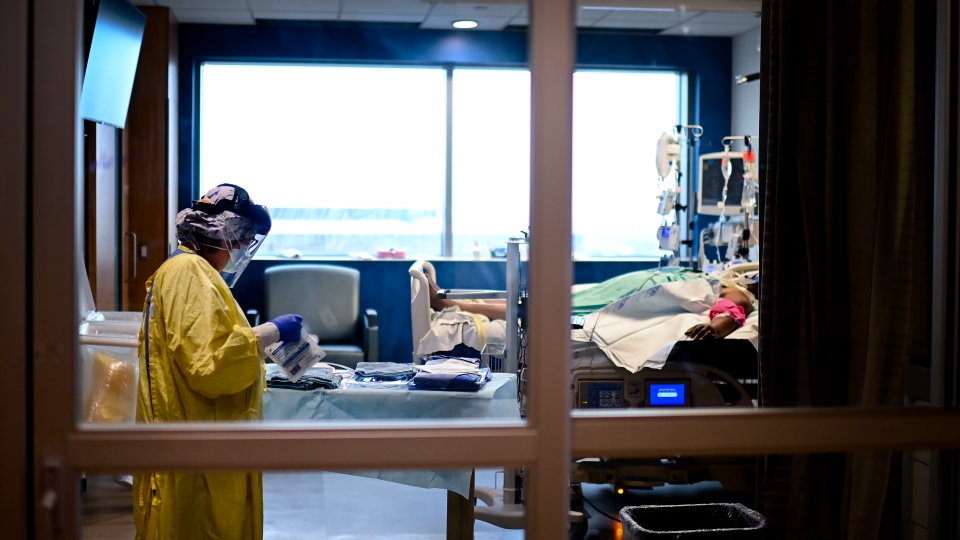
ICUs are filling up across Canada, and Chief Public Health Officer Dr. Theresa Tam says compared with the week before, there has been a 24 per cent increase in hospitalizations and 21 per cent increase in ICU admissions.
But here is some good news: COVID-19 is less deadly than it was a year ago.
The number of deaths has been increasing for five straight weeks, with the pandemic now officially claiming more than three million lives. But the deaths are not increasing at the same rate as cases and hospitalizations.
While daily new cases are seven to eight times higher than they were a year ago, and daily new hospitalizations about twice as high, the number of new deaths announced every day is less than half of what it was this time last April.
Canada is not the only place where this is occurring — a mathematical study that came out in March found that the United States and Europe saw a drop in mortality after their first waves.
Dr. Jamie Spiegelman, a critical care doctor at Humber River Hospital in Ontario, told CTV News we won’t know for sure until the third wave is over, but it appears that a smaller percentage of patients are dying than in previous waves.
“We are seeing increased survival rate during this third wave compared to the first and second wave,” he said.
But why?
There are several factors, experts say, starting with younger patients.
In the first weeks of the pandemic, the virus tore through assisted-living facilities and nursing homes, where lots of vulnerable elderly people lived. As a result, the death count skyrocketed.
But as the pandemic progressed, the virus spread in places like bars, college campuses and essential workplaces staffed by younger people, meaning many of those becoming infected were less vulnerable to severe illness.
“These patients tend to be younger working people that we're seeing during this third wave,” Spiegelman said. “And because they're healthier, they have more reserves, they tend to survive the therapies that we provide to them in the hospital as well as in the ICU.”
The number of younger people contracting the virus continues to grow, contributing to the rise in overall cases, and partially explaining the lower death rate.
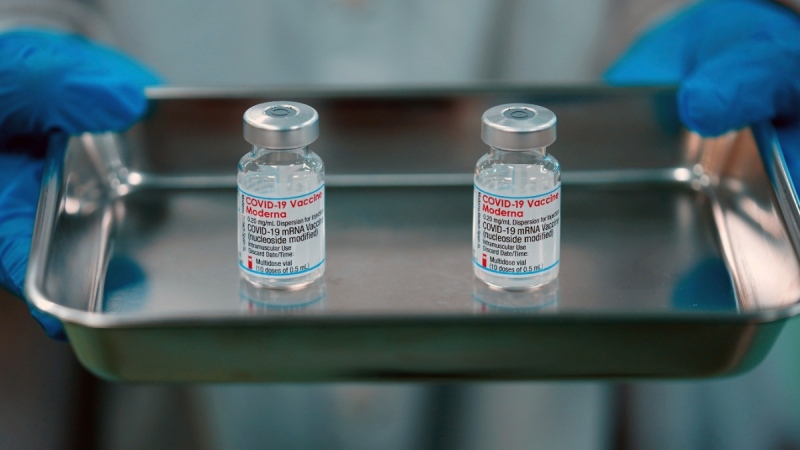
Dr. Peter Juni, professor of medicine and epidemiology at the University of Toronto and the scientific director of the Ontario COVID-19 Science Advisory table, told CTV News that the first phases of the vaccine rollout were instrumental in lowering the death rate.
“It's really making a tremendous difference that we put all our eggs into one basket when vaccinating [in] long-term care homes,” he said. “You need to be aware of that [in] wave one and wave two, 55 per cent of all deaths happened in long-term care homes, and that's the part of the pandemic we now have on the control.”
Spiegelman added that because it’s been a year since the pandemic started, and COVID-19 has been circulating for a while, it’s possible some patients also have a small degree of immunity that was built up by contracting COVID-19 earlier and not realizing it, or being exposed earlier.
In ICUs, strategies are also shifting in terms of treatment.
“The major factor that us as physicians have been able to really change in terms of outcomes is the therapies that we offer patients,” Spiegelman said.
He explained that ventilators were used more early on in the pandemic, with patients being put on a ventilator as soon as oxygen levels went down to a certain point.
“What we've learned, however, was that a lot of these patients do not need to be on ventilator early,” he said.
Other strategies, such as steroids, putting the patient in a prone position, giving patients high flow oxygen, or using machines that use “positive pressure to help you breathe,” can let doctors delay the use of a ventilator.
“We know intubating patients and putting patient[s] on a ventilator saves people's lives. There's no question about that,” Spiegelman said. “However, there are also negative effects of that in terms of having lung injury, needing heavy sedation and having a breathing tube in your mouth.
“We've learned that if we delay that enough some patients do recover to a point where they don't need to be on a ventilator and I think that does save people's lives.”
Public health measures may also be a factor in the lower death rate we’re currently seeing.
While masks and social distancing can’t always prevent 100 per cent of exposure to COVID-19, they can reduce the amount of viral particles a person is exposed to.
They will then carry a smaller viral load in their systems, making them less likely to become severely ill.
And in the rare case that a person who has been vaccinated contracts the virus, the protection provided by the vaccine will prevent them from developing a serious illness.
Experts say that although we have been seeing this lower death rate the situation is so precarious, the gains in survival could quickly disappear.
“The worst case scenario is that our ICUs are so tremendously at capacity and over capacity that we need to make […] triage decisions, and this will invariably then also increase death rates,” Juni said.
Spiegelman said that in his ICU, there are currently around 30 COVID-19 patients on “some form of life support.”
In Toronto, the University Health Network is asking all hospitals with ICUs to free up beds by end of April or early May by redeploying internal staff.
Juni added that deaths are “lagging indicators” as well, and that the deaths being reported today are not people who were admitted to hospital today.
“What we first see, of course, is the case numbers, next come hospitalizations, […] then ICU occupancy goes up, and in the end […] we start to see our numbers of deaths raising,” he said. “We have higher death rates than a few weeks ago, and that's now an indicator that this will continue to raise.”
And while more patients are surviving, it’s important to remember that many of those who survive their initial bout with the disease go on to experience mysterious and sometimes disabling symptoms for months.
“We have long COVID in perhaps 25 to 30 per cent of reported cases,” Juni said. “That's thousands of people who will have symptoms for months and months.
“So we really need to get these numbers down.”