TORONTO -- At least 1,460 Canadians have died from opioid-related overdoses in the first half of 2017 -- a number that's expected to rise, as not all provinces have reported final data for the period, the Public Health Agency of Canada said Monday.
Dr. Theresa Tam, chief public health officer of Canada, said Ontario, Quebec and Manitoba are yet to report all of their opioid-related overdose deaths for the first half of the year.
But based on figures reported by the other provinces and territories, Tam said the number of overdose deaths are on pace to surpass 4,000 by the end of the year -- far above last year's tally of 2,861 opioid-related fatalities.
"It's an extremely complex whole-of-society issue that we're dealing with. This is a national public health crisis," Canada's top doctor said in an interview from Ottawa.
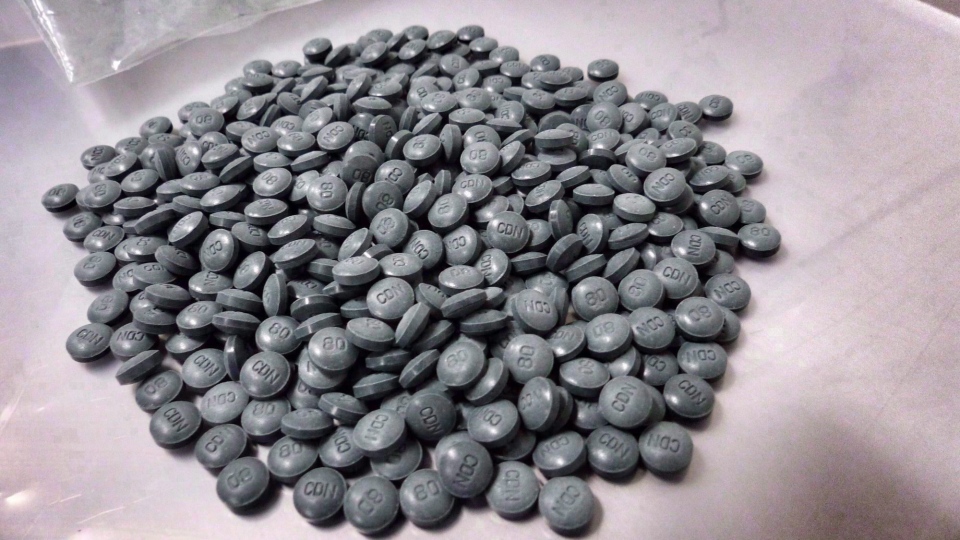
"First and foremost there is a very toxic drug supply," she said, referring to illicit fentanyl, a powerful and potentially deadly opioid that is increasingly finding its way into street drugs across the country.
"So we've seen the proportion of fentanyl as part of the opioid-related deaths go up 75 per cent now, and that's increased compared to last year," she said.
In 2016, illicit fentanyl was implicated in 53 per cent of all opioid overdose deaths.
"It's such a toxic drug that there is no second chance," Tam said. "So people may die at the first exposure to fentanyl and we can't even get them to treatment."
While British Columbia and Alberta have been hardest hit by fentanyl-related overdose deaths, Ontario is also seeing the opioid seeping into its street drug supplies, often with fatal outcomes.
Tam said no province or territory is immune to a fentanyl-contaminated drug supply -- "it could hit all other areas of Canada and that's why it's so concerning."
The PHAC report showed three-quarters of opioid-related deaths occurred among males, with the highest proportion (28 per cent) clustered among Canadians aged 30 to 39.
A number of measures have been implemented to counteract the growing number of overdose deaths, including supervised injection sites for drug users and increased access to the rescue medication naloxone.
But Tam said it's likely too early for those programs to have had much effect in reducing the number of deaths, as many safe-injection sites, for instance, have only recently begun operating.
All levels of government need to work together to improve access to treatment for people struggling under the yoke of drug abuse, she said.
"This crisis is really based on some very difficult societal challenges, including stigma to the persons who have problematic substance use and also some of the social economic factors such as homelessness and poverty," Tam said.
"So this is an extremely complex issue and as we move into 2018, we really need the whole of Canada to be prepared."